All About Mucormycosis or Black Fungus: A Double Danger For COVID-19 Patients In India

India was already battling with the deadly second wave of COVID-19, but another hurdle aka Mucormycosis stumbled upon its door. Reportedly, many states are observing the cases of Black Fungus in their citizens. The disease is lethal and has the potential to damage the eyes of the infected patients permanently.
The country is already struggling in managing the medical health infrastructure and medical supplies, but with the introduction of this new virus, another endangerment is emerging for us. The disease has already spread in Gujrat and Maharashtra affecting hundreds of people. Scientists all around the world are explaining the perniciousness of this disease. Now, the question is, how the already failing government manages the arrival of this new disease?
The COVID-19 pandemic already destructed the country’s function at every level. While the millions of people were dying daily due to the lack of oxygen and hospital beds, the government, on the other hand, left no stone unturned to show a bare-face to its citizens. The vaccination drive is running at an ever slow pace across the country, wherein millions of people are feeling ‘left out’ as they can’t book their vaccine slots. But due to the unfair management and irresponsible behavior of the government, they won’t be able to get their vaccine shots which eventually increases the chance of getting severely infected by the double whammy of diseases.
What is Mucormycosis or Black Fungus?
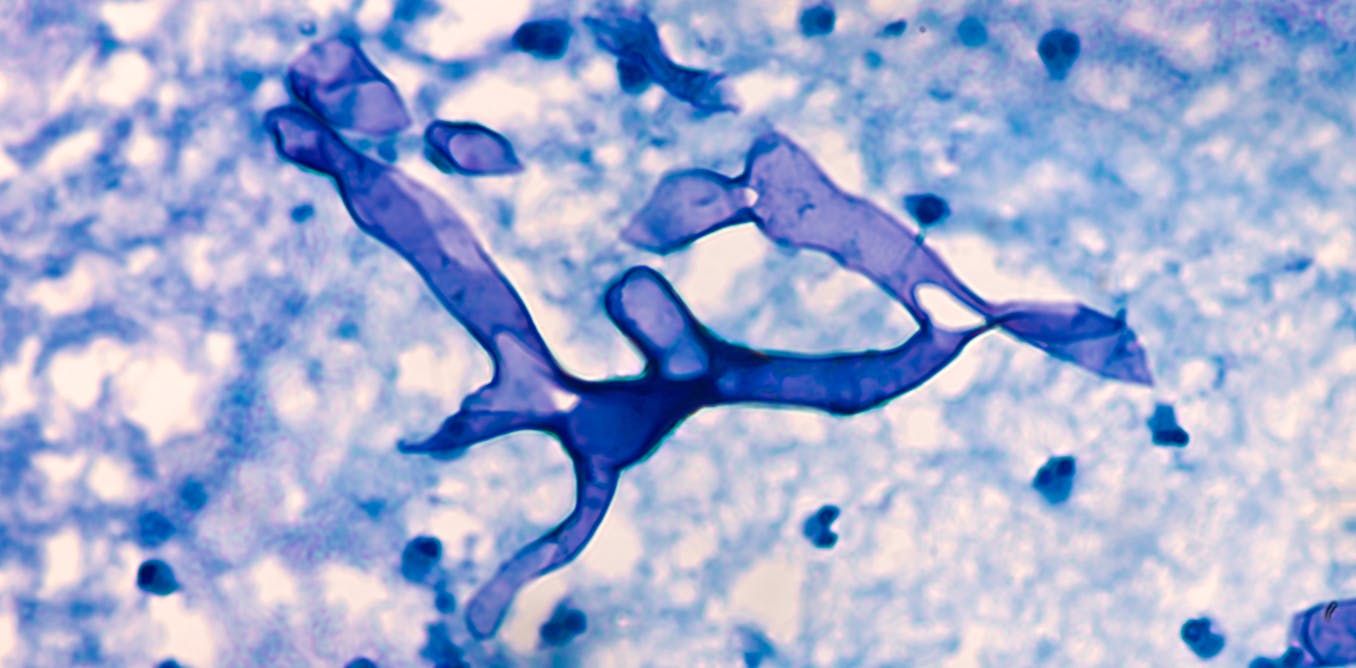
Mucormycosis is a serious but rare disease caused by a group of fungi called ‘Mucormycetes’. Mucormycetes live throughout nature and are found everywhere in nature. It can affect areas that can be pulled – through the nose/eye/lungs. If the fungal spored enters via a wound or skin, then it infects the tissue locally, but if it enters from the sinuses, it can severely affect the eyes and brain.
Poor diabetes management is a major cause of increasing numbers, especially after Covid. Also, patients with immunosuppression programs, or those that have been implanted, put on immunosuppressants, or have been on a ventilator for a long time, are at greater risk.
Formerly known as ‘zygomycosis’, this fungal disease is caused by a group of funguses that belongs to the family “Mucorales”. It is commonly found in tropical and subtropical regions. Apophysomyces are another kind of this virus that is found in India. Rhizopus oryzae is one of the families of this fungus that causes the infection in humans. This fungus has a black/brown appearance and grows fast in laboratories. Usually found in soils, this fungus can also grow on dead and decaying matter.
How do humans contact Mucormycosis?
People with damaged tissue and weak immune system are more susceptible to get infected by the black fungus as it is an opportunistic fungus. Corticosteroids, a drug that suppresses the immune system can weaken it and can lead to other immunocompromising (conditions that make the human immune system weak by attacking it) conditions, just like in cancer. Trauma, accidents, and injury lead to damaged tissue. Mucormycosis has 3 modes of propagation:
- Propagation through the air: By inhaling the spores
- Contamination: Entering the body through wounds and cuts
- Mechanical propagation: By swallowing the spores through food
Out of these three, the air mode of propagation is the most common. You would be shocked to know that our body inhales various types of spores every day, but our body is strong enough to fight against those foreign spores. When the lungs are damaged and the immune system is suppressed, as is the case with patients with severe COVID, these cells can grow in our airways or sinuses and invade our body tissues.
Mucormycosis can be seen in the lungs, but the nose and nerves are the most common cause of infection with mucormycosis. From there it can spread to the eyes, which can cause blindness, or brain damage, causing headaches or rashes. The disease affects the skin too by entering the body through wounds.
Why Mucormycosis outbreak suddenly emerged in India?
A very few counties have reported Mucormycosis cases. Australia, UK, USA, etc on the other hand has not reported any cases of the disease so far. Why is it so? So, let us analyze this situation.
Mucormycosis was already prevailing in India way before the COVID-19 pandemic. In India, every 14 in 1,00,000 people get affected by the fungus. Whereas in Australia, merely 0.06 out of 1,00,000 people get affected by it. In the other parts of the world, the Mucormycosis cases emerged from the contaminated hospital linen, packaged foods, and medicines. But in India, the case is not likewise. The Mucorales are spurting from natural sources like soil, rotted meat, animals, birds, air, water, moist conditions, construction sites, etc.
Diabetic patients at greater risk of getting infected with Mucormycosis
People with diabetes have a comparatively weaker immune system which makes it tough for the body to fight against the fungus. When diabetes is poorly controlled and the blood sugar is high, the tissues become acidic – a good place for the Mucorales fungus to grow. It was identified as a risk factor for mucormycosis in India (where diabetes is highly prevalent and often uncontrolled) and worldwide before the COVID epidemic. In all cases of mucormycosis published in scientific journals worldwide between 2000-2017, diabetes was detected in 40% of cases.
97% patients had diabetes, and more than 67% of the case was poorly controlled reveals a survey. Hence both COVID and mucormycosis affect patients having diabetes and weak immune systems. So start taking vitamin C pills, and approach a healthy lifestyle!
Patients suffering from diabetes and obesity have to take corticosteroids to combat the COVID-19 infections. As mentioned earlier, Corticosteroids weakens the immune system, and hence the black fungus attacks them. It all adds up and results in many critical complications in diabetic patients. So in India, treatment of diabetic COVID-19 patients with corticosteroids, damage to tissues through COVID, and a high rate of diabetic patients along with the contaminated environment contributes to a high rate of Mucormycosis cases.

How to prevent Mucormycosis infection?
The most effective way to prevent black fungus is to cover your face when you are outdoors, especially in gardens and dusty areas or where you may come in contact with rotten rubbish or food. Second, wear clothing that does not expose your skin or reveal your appearance as little as possible. Most importantly, for people with diabetes and other vulnerable people, control of blood sugar and blood glucose levels is necessary. People given steroids should be monitored regularly and the dose should be reduced in consultation with your doctor.




