PM-JAY: Five Insurers to Refund Rs 458 Crore for Low Claims Ratio in 2023

PM-JAY: Five Insurers to Refund Rs 458 Crore for Low Claims Ratio in 2023
In Maharashtra, the National Insurance Company must return Rs 214 crore, while United India Insurance must refund Rs 72 crore under the CAG audit of PM-JAY from 2018–19 to June 2022.
Five general insurance companies that offer health insurance coverage through the Pradhan Mantri Jan Arogya Yojana (PM-JAY) have been flagged by the Comptroller and Auditor General (CAG) as needing to refund premiums totalling Rs. 458 crores because they failed to meet the required claim-to-premium ratio in five states and one Union Territory.

In Maharashtra, the National Insurance Company must return Rs 214 crore, while United India Insurance must refund Rs 72 crore under the CAG audit of PM-JAY from 2018–19 to June 2022.
In Gujarat, Oriental Insurance must return Rs. 55 crore, while United India Insurance must refund Rs. 111 crore. For free, PMJAY provides health coverage of Rs 5,000 per year to 107 million low-income households nationwide, or about the poorest 40% of the population. According to the insurance model, the Centre and the states split the expense of the premiums in a 6:4 ratio.
100% of the excess shall be returned by the insurer to the state health agency within 30 days after adjusting a certain amount for administration costs (which range from 10% to 20%) and after all claims have been resolved. The insurers must pay 1% weekly interest on the return amount after 30 days.
As of November 2022, the trust and insurance models have resolved 35.7 million claims totalling Rs 42,433 crore. The six brownfield States of Andhra Pradesh, Arunachal Pradesh, Rajasthan, Karnataka, Maharashtra, and Tamil Nadu received claims totalling Rs 22,620 crore (53.3%). These States process the allegations using their IT platforms, which they input through an Application Programming Interface (API) into PMJAY’s Transaction Management System.

“Without segregation of PMJAY beneficiaries in such cases, there is a possibility that PMJAY will overlap with state-specific schemes,” CAG stated.
The National Health Agency, the PM-JAY’s central agency, responded that it would ask all states and UTs implementing the programme in insurance or mixed mode (insurance and trust models) for a final settlement declaration.
The Beneficiary Identification System (BIS) database has 7,49,820 beneficiaries associated with just one cellphone number (9999999999), among other problems that the CAG brought up. A second cell number (8888888888) is also associated with 1,39,300 recipients. Despite agreeing with the audit’s findings, NHA said this problem should be remedied once BIS 2.0 is implemented.
Furthermore, the BIS 2.0 system is set up to prevent more households from using a single mobile number than a specific threshold. This will end the practice of entering “random numbers,” which account for most inconsistent mobile number situations.
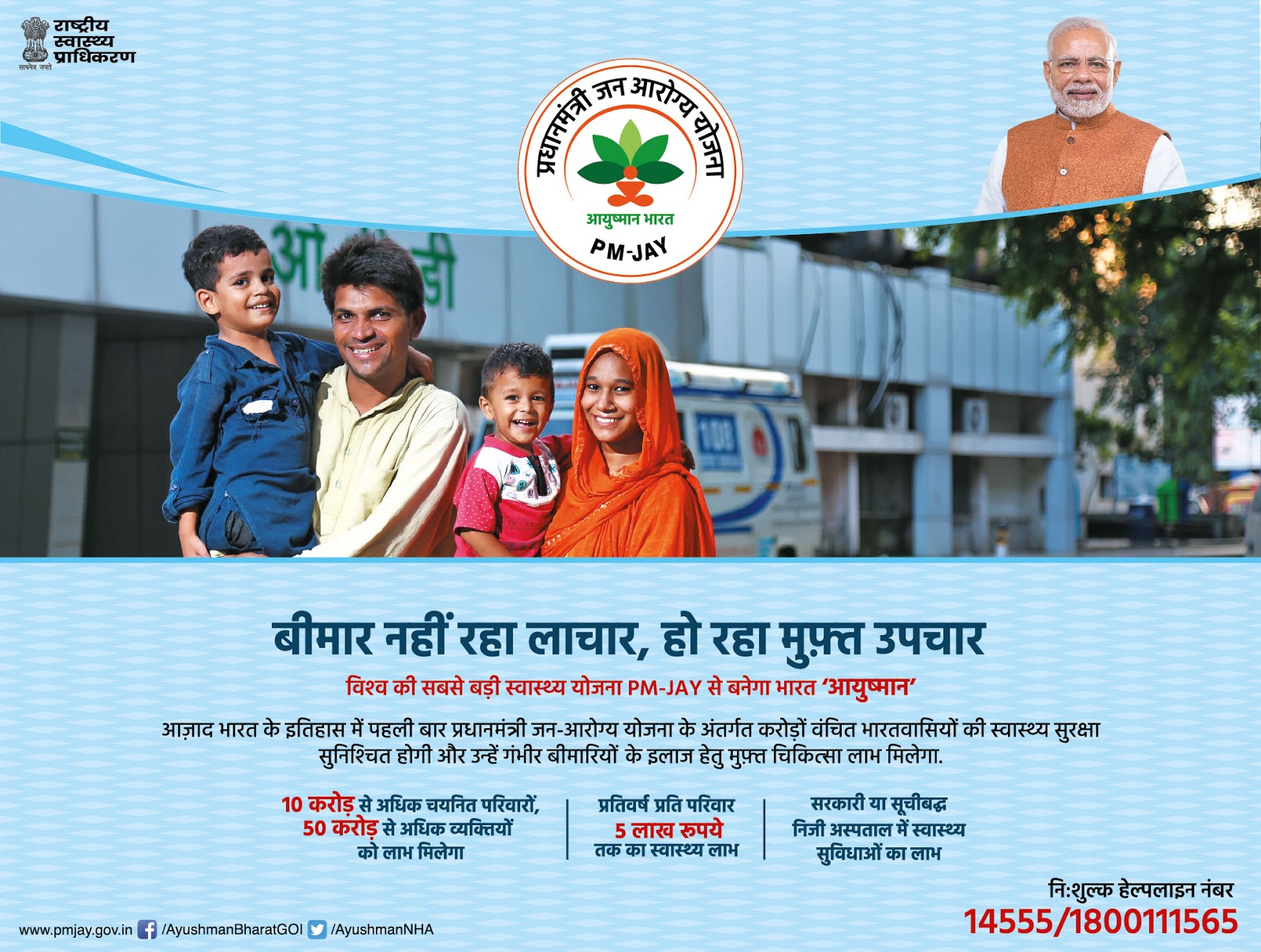
The Pradhan Mantri Jan Arogya Yojana (PM-JAY) is a flagship health insurance initiative launched by the Government of India. Its objective is to provide free hospitalization benefits to the country’s poorest citizens, thus significantly reducing their financial burden due to health issues. In a recent turn of events, five insurers under PM-JAY are set to refund a whopping Rs 458 crore to the government due to their low claims ratio in 2023. This article will delve into the details of the PM-JAY initiative, the reasoning behind the refund, and its implications.
Launched under the broader umbrella of the Ayushman Bharat program, PM-JAY is often referred to as the world’s most extensive publicly-funded health insurance program. It aims to benefit over 500 million Indian citizens, offering a cover of up to Rs 5 lakh per family per year for secondary and tertiary hospitalization. The beneficiaries are identified based on a predefined criteria set, mainly targeting the socio-economically vulnerable sections of society.
In insurance terminology, the ‘claims ratio’ is a measure that indicates the proportion of insurance claims paid by the insurer to the premiums earned during a specific period. A low claims ratio means that the insurer has paid less in claims than the premium they collected.
For the year 2023, it was found that five insurers under the PM-JAY initiative had a significantly lower claims ratio than what was stipulated in their agreement with the government. This meant that many of the premiums collected from the government, intended for beneficiary payouts, remained unused.
Based on the agreements between the government and the insurers, if the claims ratio falls below a certain threshold, the insurers are bound to refund the difference to the government. This mechanism ensures that insurance companies do not unduly profit from the funds allocated for public health and that these funds can be reallocated or used for other health-related initiatives.
The refund, while ensuring accountability, also boosts public trust. It reinforces the idea that the government is keeping a close watch on the system and is committed to preventing undue profits at the public’s expense.
Such instances of refunds can impact the future pricing of health insurance premiums under the scheme. Insurers might become more competitive and realistic in their premium calculations. One reason for the low claims ratio could be that many beneficiaries must know how to claim the benefits. This underscores the need for better outreach and awareness programs.
There’s a possibility that specific bureaucratic processes or technical issues might be causing hindrances in claim processing. The government and insurers may need to investigate and rectify systemic such problems.

While the refund from the insurers underscores the robust checks and balances in PM-JAY, it also highlights the need for continuous improvements in beneficiary outreach and systemic efficiency. With the government’s commitment to ensuring the health of its most vulnerable citizens, the PM-JAY scheme is expected to continue to evolve and benefit millions in the country.




