India’s Antibiotic Apocalypse: The Hidden Killer Draining Lives And Resources
ICMR's findings reveal the economic and health implications of drug-resistant infections in India, urging systemic and individual action.

One of the most significant risks to world health is antibiotic resistance. In India, it has primarily become a substantial financial and medical problem. A recent study by the Indian Council of Medical Research revealed that drug-resistant infections accounted for a phenomenal 33% increase in the cost of healthcare. This is not merely a threat to the individual’s health but also to the family and the entire healthcare system through economic burdens.
Understanding Drug Resistance
In drug resistance, pathogens like bacteria, viruses, fungi, and parasites resist the medicines prepared to kill or stop them. This has been more visible with antibiotics. With time, microbes adapt themselves, causing medicines to become useless and resulting in prolonged infections.
Because India has a high population density and infectious diseases occur in relatively more significant proportions, it is significantly exposed to antibiotic resistance effects. The overuse, misuse, and self-administration of antibiotics accelerate the development of resistance among pathogens.
ICMR Study: Key Findings
The ICMR‘s findings expose the severe economic and medical costs of drug-resistant infections:

- Increased Medical Costs: According to the study, there is an increase of 33% in healthcare expenditure from patients or families suffering from drug-resistant infections. All these additional expenditures are due to more extended hospitalization, higher morbidity, and expensive second or third-line drugs.
- Extended Recovery Periods: Most drug-resistant infections lead to extended recovery periods and thus increased periods of illness, along with additional healthcare interventions.
- Higher Mortality Rates: Patients with drug-resistant infections face a greater risk of complications and death, particularly in cases involving sepsis, pneumonia, or bloodstream infections.
- Economic Burden on Families: For families, that includes direct health care costs and lost income due to prolonged illness and extra caregiving duties. For people with low incomes in India, those costs lead to catastrophic health expenditures for many.
- Antibiotic Overuse and Misuse: The paper further notes that misuse and overuse of antibiotics—often without prescription—is one of the key factors behind resistance. This includes easy availability of the counter and broad-spectrum antibiotics for minor ailments.
Major Drivers of Antibiotic Resistance in India
The rise in drug-resistant infections can be attributed to a combination of behavioural, systemic, and policy-related factors:
- Self-Medication: An overwhelming number of people buy antibiotics over the counter and use incorrect dosages or do not complete the entire course.
- Unregulated Sales: The government regulations have failed to prevent the rampant sale of antibiotics without prescriptions; they are highly available in most rural areas.
- Over-Prescription: Physicians, under compulsion to make quick fixes, over-prescribe antibiotics.
- Agricultural Use: In the livestock sector, antibiotics promote growth and prevent infections, creating resistant strains that can be transferred to humans through food.
- Poor Sanitation and Hygiene: A lack of sanitation and access to clean water enhances the spread of infections, increasing the need for more antibiotics.
- Healthcare-Associated Infections: This is a source of drug-resistant infections for all hospitals and clinics, primarily in cases where the infection control measures are poor.

Implications for Public Health
Significant public health threat in the rise of drug-resistant diseases:
- Reversal of Medical Advancements: Conditions previously treatable, such as tuberculosis, urinary tract infections, and pneumonia, are becoming harder to manage.
- Increased Healthcare Demand: Overburdened healthcare facilities face challenges in managing the growing number of resistant cases.
- Threat to Surgical Outcomes: Antibiotics are critical in preventing infections post-surgery. Resistance jeopardizes these outcomes, leading to complications.
- Global Implications: Given that India is now the biggest hub for medical tourism, its high resistance levels would cross borders, potentially destabilizing healthcare in other nations as well.
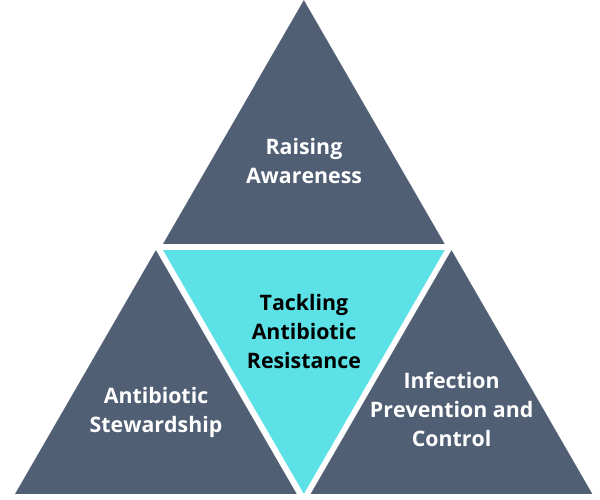
Recommendations to Tackle Antibiotic Resistance
The prevention of drug-resistant infections must be multi-faceted at the individual, organizational, and policy levels. Some recommendations from the ICMR study include:
- Public Awareness Campaigns:
- Public enlightenment of the dangers of antibiotic misuse and the importance of finishing courses prescribed.
- Educate people on the dangers of self-medication.
- Strengthening Prescription Regulations:
- Enforce stricter regulations to prevent over-the-counter sales of antibiotics.
- Monitor prescription practices and detect misuse patterns by putting in place monitoring systems.
- Improved Infection Control:
- Boost infection control and prevention strategies in clinics and hospitals.
- Encourage regular hand hygiene, sterilization of medical equipment, and isolation of infected patients.
- Promoting Rational Antibiotic Use:
- Training health practitioners to use antibiotics only when necessary.
- Promote the use of diagnostic tests to diagnose infections before administering antibiotics.
- Reducing Agricultural Antibiotic Usage:
- Regulate and limit the use of antibiotics in livestock.
- Encourage alternatives such as vaccination and improved animal husbandry practices.
- Investment in Research and Development:
- Support new antibiotics and other options.
- Quick diagnostic procedures to differentiate between viral and bacterial illnesses.
- Enhancing Surveillance:
- Develop a surveillance system that monitors resistance patterns for treatment protocols.
- Collaborate with global networks to share data and strategies.
Steps for Individuals to Protect Themselves
While systemic changes are necessary, people can take precautions to minimize the risk of acquiring drug-resistant infections:
- Avoid Self-Medication: Always see a doctor before taking antibiotics, and never buy them from a pharmacy over the counter.
- Complete Prescribed Courses: Even if symptoms improve, complete the entire course of antibiotics to eradicate the infection.
- Practice Good Hygiene: Wash hands frequently, use safe food practices, and keep things clean to minimize the chances of infections.
- Vaccinations: Get vaccinated against infections that might need antibiotic treatment.
- Support Sustainable Practices: Buy food products from farms that have restricted the use of antibiotics.
Conclusion
The ICMR’s findings serve as a wake-up call for the fact that India is gradually facing the emergent crisis of drug-resistant infections. A 33% hike in medicine costs has profound economic and health implications. No single party—from policymakers to enact regulations to individuals taking conscious antibiotic use precautions—can do everything alone to eliminate antibiotic resistance, but everyone collectively can do that.
India should implement the recommended strategies to curb the incidence of drug-resistant infections. This requires immediate and prompt action to ensure that common infections become untreatable, and the progress of modern medicine is not undermined in the future.




