Indians Have Lost immunity Against MonkeyPox. Are we expecting Another Pandemic in India 2022?

Indians Have Lost immunity Against MonkeyPox. Are we expecting Another Pandemic in India 2022?
The top monkeypox expert at the (WHO) World Health Organization asserted she doesn’t predict the numerous Indians that have reported so far to turn into the next pandemic. However, she has acknowledged that there are still many unknown variables about the disease, how it’s extending and whether the disqualification of mass smallpox vaccination decades ago may be hastening its spread.
Dr. Rosamund Lewis of the World Health Organization has noted it was essential to emphasize that the vast majority of instances seen in dozens of nations around the world are in gay, bisexual, or men who have intercourse with men so that scientists can continue to study the issue and populations at risk can take precautions, in a public week so.
 “There’s critical to explain this because it tends to be an increase in the form of transmission that has hitherto gone unnoticed,” Lewis, WHO’s the technical lead on monkeypox, said.
“There’s critical to explain this because it tends to be an increase in the form of transmission that has hitherto gone unnoticed,” Lewis, WHO’s the technical lead on monkeypox, said.
Nonetheless, she cautioned that anyone, regardless of sex, is in danger of contracting the disease.
Other scientists have suggested that the disease’s emergence in homosexual and bisexual men may have been coincidental and that it might quickly spread to other groups if not addressed.
Following an uptick in monkeypox cases in certain foreign nations, a medical professional on Saturday urged people to keep an eye on the disease’s progress while simultaneously warning them not to panic.
(NCDC) The National Center for Disease Control and the Indian Council of Medical Research (ICMR) was given notice on Friday by the Centre, asking them to keep a close eye on the situation in regard to the monkeypox cases abroad.
“Everything should be treated with caution. And while we should remain vigilant and do not need to become alarmed. We need to figure out how it’s progressing and how many people are affected. Thankfully, it isn’t as bad as smallpox. “ANI spoke with Dr. Ishwar Gilada, an infectious diseases researcher and HIV/STD consultant.
“We currently have no method of knowing how many individuals are dying and whether or not they have received any treatment. We don’t know what the treatment is, but it’s possible that the smallpox vaccination could be employed. It could be utilized as a medication, but we don’t know for sure, “He said. The transmission of the monkeypox virus is uncertain.
Lewis has said it’s unclear if monkeypox can spread through intercourse or by intimate contact between people who engage in sexual activity. The risk to the general people is “minimal.”
“It’s unclear whether this infection is using a novel way of transmission, but it’s apparent that it’s still using its well-known propagation, which is close, body contact,” Lewis explained.
Monkeypox is transferred by immediate physical contact with an infected person, their clothing, or their bedsheets.
She also cautioned that among the latest occurrences, there is a more enormous number of persons with fewer lesions, which are more confined in the vaginal region and can be challenging to see.
“You may have these blemishes for two to four weeks, and they may not be obvious to others, but you could still be infectious,” says the doctor “she stated. Monkeypox is a zoonotic virus, which means that it spreads from animals to humans. We have no idea whether COVID-19 is Zoonotic or not.
However, HIV is a zoonotic virus that began as a monkey virus known as simian immunodeficiency virus or SIV, and subsequently evolved into HIV,” he explained.

“So, this is monkeypox, or monkeypox, which was initially identified in monkeys exclusively in the rainforest region of Central Africa about 1958. However, it is possible that it has since spread to humans, but the first occurrences were only discovered in the 1980s,” Dr. Gilada remarked.
“Basically, what we are now worrying about is a lot of new diseases will be viral infections,” the specialist added, detailing the type of virus and the therapy provision. Infections are divided into four categories: microbial, fungal, parasitic, and viral.”
“Antibiotics are pretty effective against bacteria, antifungal agents are very efficient against fungus, and anti-parasitic agents are very effective. Because there are no potent post-exposure prophylaxis and viruses are very different, such as RNA and DNA viruses, they are adaptable, change their shape, have unique clades, multiple versions, sub-variants, and it becomes very tough to locate antivirals “Dr. Gilada explained.
Meanwhile, the World Health Organization (WHO) has examined 80 incidents of monkeypox in 11 countries and says it is working to know the extent and source of the outbreak.
The WHO stated in a statement released on Friday that the virus is prevalent in some large mammals in several nations, causing outbreaks among locals and visitors on occasion.
Monkeypox is an infectious zoonosis (a virus passed from animals to humans) with symptoms that are strikingly similar to those used in smallpox patients in the past. However, it is less severe clinically.
Monkeypox is characterized by a fever, rash, and swollen lymph nodes, according to the World Health Organization, and can result in various medical consequences. Monkeypox is generally a self-limiting condition that lasts between 2 and 4 weeks.

What exactly is monkeypox?
Monkeypox is a virus related to smallpox but has less severe symptoms. According to the National Center for Illness Control, it is an endemic viral disease that occurs primarily in tropical forested areas of Central and West Africa and is sometimes transported to other regions (NCDC).
The incubation phase lasts from five to three weeks. Most of the patients recover in four to six weeks without the need for hospitalization.
What is the origin of the name monkeypox?

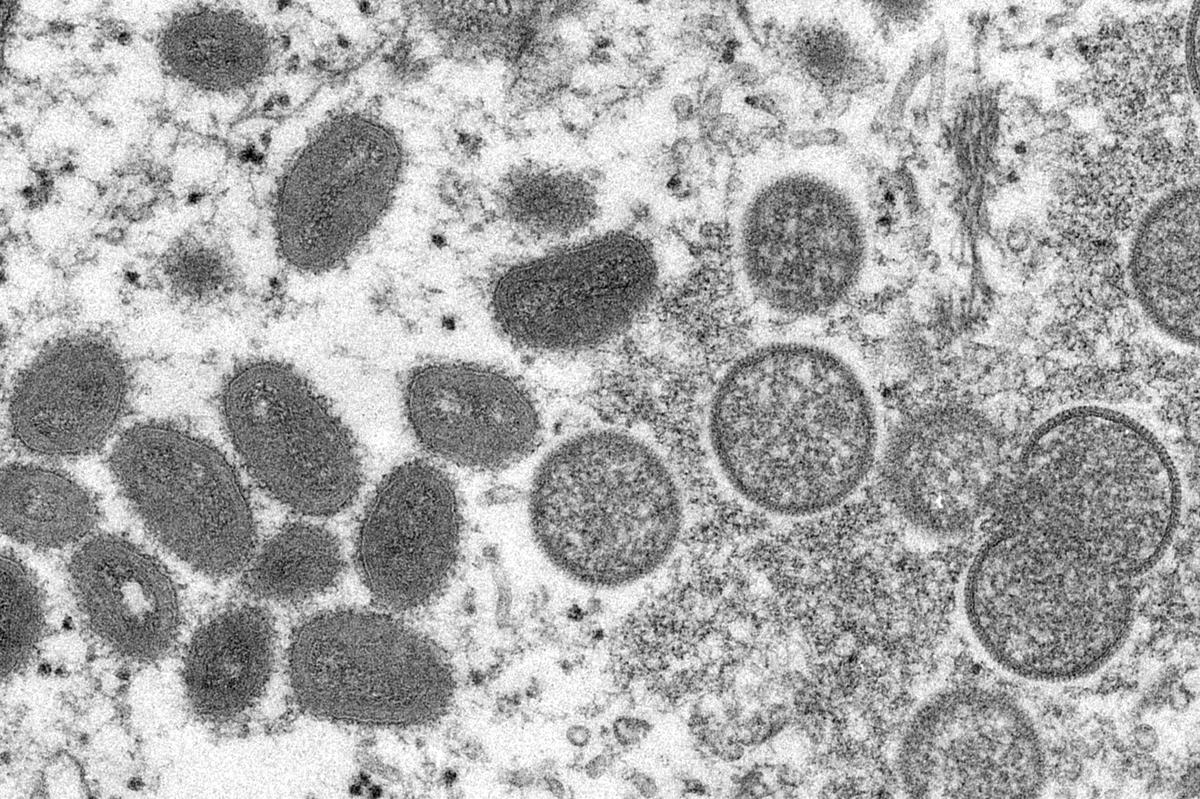
The disease is known as monkeypox since it was discovered in 1958 in a colony of monkeys held for research. It was only in 1970 that it was found in humans.
Outside of Central and West Africa, infections are uncommon, though two cases were reported in the United States last year, both in visitors arriving from Nigeria. Here are five major things to be aware of about all these life-threatening illnesses.
1. It’s caused by a virus that’s similar to smallpox.
The virus that causes monkeypox is closely linked to smallpox, which has since been wiped from the world. Both belong to the Orthopoxvirus genus, which is part of the Poxviridae family. In 1958, outbreaks of the disorder pox were detected in monkeys kept captive for research. It was initially discovered in humans in the Democratic Republic of the Congo (DRC) in 1970 and is now found throughout Central and West Africa.
The World Health Organization (WHO) recorded 4,594 probable monkeypox cases in 2020, with 171 deaths (case fatality ratio of 3.7 percent ). Because confirmation needs PCR testing, which is not readily available in endemic areas, they are characterized as suspected.
2. Pustules appear all over the body.
Symptoms usually develop five to thirteen days after infection, but they can take up to twenty-one days. Fever, muscular discomfort, headache, swollen lymph nodes, chills, and tiredness are common early symptoms. Following the onset of a fever, a rash appears, initially concentrating on the face, hands, and feet before migrating to other parts of the body. It can infect the mouth, the genitals, and the cornea, among other places. The rash spreads until it produces a scab, which breaks off, and significant chunks of skin can sometimes peel off the body.
Although symptoms usually go away after a month, one in every ten instances might be fatal. Children are especially vulnerable.

3. PCR testing is required for diagnosis.
Because rashes can be found in various diseases, including chickenpox and measles, which suggests diagnosis when a diagnosis is required. They claim that this can only be done with PCR testing because orthopoxviruses create antigens and elicit antibodies that could be mistaken for those of other viruses. Hence, analysis of these cannot determine whether the virus is monkeypox.
4. It can be passed from person to person through intimate contact.
Infected wild animals, such as rats and primates, carry the virus to humans in the Central and West African rainforests, although human-to-human transmission is also possible.
Transmission is limited to close proximity, similar to infections like Ebola, and occurs by contact with blisters, body fluids, coughing and sneezing, or infected objects such as mattresses or clothing.
5. There is no cure at the moment, but we do have a (very old) vaccination.
There is currently no WHO-recommended treatment for monkeypox. However, antivirals such as tecovirimat have been approved to tackle orthopoxviruses.
The smallpox vaccination was crucial in eradicating smallpox centuries back, and it can also prevent monkeypox with an efficacy of 85 percent. The first-generation smallpox vaccines, on the other hand, are no longer accessible to the general population. In 2019, a novel vaccinia-based vaccination for the protection of smallpox and monkeypox was licensed, but it is still not widely available.
Do monkeypox, and chickenpox/smallpox have anything in common?
“Monkeypox is a contagious disease that is comparable to chickenpox or smallpox. It is, however, less severe than smallpox. Chickenpox, smallpox, and tertiary syphilis can all cause rashes “Dr. Saranya CK, Senior Resident, Government Medical College, Konni, Department of Microbiology.
Will those who have already had chickenpox or smallpox be immune to this virus?
“Those who have already had chickenpox do not have immunity against monkeypox. Those who received the smallpox vaccine, on the other hand, are immune to monkeypox infection. Vaccinations versus smallpox were effective, but because smallpox immunization was discontinued after the disease was eradicated, persons may be more sensitive to monkeypox infection, “Dr. Saranya stated the following.
Is it possible to die from monkeypox?
Monkeypox symptoms tend to disappear on their own after a few weeks, but they might cause medical issues and even death for some people.
What is the method of transmission?
Monkeypox can spread from people to humans and from animals to humans. The virus is transmitted from damaged skin, the respiratory tract, or nasal passages (even if they are not apparent) (eyes, nose, or mouth).
Animal-to-human transmission from an animal to a human can happen through a bite, a scratch, or making interaction with bodily fluids. It can also occur if a user interacts with virus-infected objects. Human-to-human transmission is assumed to be predominantly accomplished through large respiratory droplets, necessitating sustained close contact.
It can also be spread through direct touch with body fluids or disease material and indirect contact with tumor content, such as through an infected person’s contaminated clothing.
What is the origin of monkeypox?
Last week, a top WHO consultant claimed the outbreak, which has spread across Europe, the United States, Israel, Australia, and beyond, was most likely caused by sex at two lately raves in Spain and Belgium.
This is a dramatic divergence from the infection’s traditional distribution pattern in central and western Africa, where individuals are primarily infected by animals such as wild rats and primates, and outbreaks haven’t crossed borders.
What is the best method to tell whether you have monkeypox?
Fever, body pains, uneasiness, chills, and weariness are the most common symptoms observed in monkeypox. A rash and ulcers on the face and hands may appear in people who have a more severe condition, and these lesions can travel to other areas of the body. In the present outbreak, no deaths have been reported.
While past monkeypox outbreaks in Central and Western Africa had been reasonably controlled, WHO’s Lewis said it was unclear whether people might spread monkeypox without manifestations or if the disease could be transferred through the air, like measles or COVID-19.
Monkeypox is spreading for three reasons:
Is the smallpox vaccine effective in preventing monkeypox? Thus according to National Geographic, the abolition of smallpox is a significant factor in the rise in monkeypox incidence. Smallpox was proclaimed eliminated by the World Health Organization in 1980, and vaccination against the virus was discontinued.
Many of us over 40 or 50 have a scar on our arms, mainly on the left upper arm, as a memory of the smallpox vaccination. However, most of the world’s population, particularly the younger generation, has never seen or heard of smallpox disease, let alone received a smallpox vaccine. However, researchers discovered that this now-discontinued smallpox vaccination, which has adverse effects, gave 85% protection against monkeypox.
Vaccinated persons had a nearly fivefold decreased risk of contracting monkeypox than unvaccinated people, according to a 2010 study from Central Congo. According to Nature.com, indiscriminate tree cutting is now causing problems: As deforestation increases, more people may become infected with the virus. Clearing forests for plantations and cultivation is likely to put humans near afflicted wild animals, perhaps enhancing the virus’s ability to hop species, as Ebola has shown.
The virus that causes monkeypox is evolving: In addition, a 2014 study discovered one form of the Congo Basin monkeypox virus strains with a missing gene that could be linked to a human-to-human transmission adaption.
Monkeypox currently has a stigma linked to it, with the majority of sufferers being gay: Another source of concern is the growing stigma surrounding the recent monkeypox outbreaks, as many of the illnesses have been in guys who have had intercourse with other men.
In a 2021 comment in Nature Medicine, Daniel Bausch, the board member of emerging risks and global health security at the Base for Innovative New Diagnostics in Geneva, Switzerland, wrote that if the disease is stigmatized, people may refuse to comply with contact-tracing efforts, making ring vaccination much more difficult.

Monkeypox is passed from generation to generation in a variety of ways.
Monkeypox patients are contagious when feeling unwell (typically for two to four weeks). Monkeypox can be contracted by direct physical contact with those exhibiting symptoms. The rash, biological fluids (such as fluid, pus, or bleed from skin lesions), and scabs are all extremely contagious. Clothing, blankets, towels, and things such as dining soup spoons that have been polluted with the virus as a result of sex with an infectious individual can infect others.
Infectious ulcers, lesions, and blisters in the tongue can also transfer the virus through saliva. People with close contact with a contagious person, such as Monkeypox patients, household members, and sexual partners, are to become infected.
The virus can be passed from a pregnant woman to her fetus through the placenta or from an afflicted parent to their kid through skin-to-skin contact during or after birth. It’s unclear whether those who don’t show any signs of the sickness can spread it.
Are we on the edge of another pandemic?
“Although it is not as contagious as SARS Cov-2, it does create epidemics in some areas. In some countries, it might become an epidemic. It has a lower possibility of becoming a pandemic, “Dr. Saranya stated.

Is there a link between smallpox and monkeypox?
Monkeypox is similar to smallpox, although the symptoms are less severe. Countries ceased mass immunization campaigns after smallpox was proclaimed eliminated in 1980, a move that some specialists feel may have aided the spread of monkeypox because there is now minimal broad immunity to similar diseases; smallpox immunizations are also beneficial against monkeypox.
Lewis asserted that it would be “unfortunate” if monkeypox were able to “exploit the immunity gap” left by smallpox 40 years ago, but there was still time to stop the outbreak and prevent it from spreading to new areas.
Coronavirus vs. monkeypox
The SARS-CoV-2 virus, which causes Coronavirus infection, was originally discovered in Wuhan, China, in 2019. On the other side, the monkeypox virus was initially discovered in 1958 and is more widespread in West and Central Africa. It has now extended to 15 countries. “The situation is developing, and WHO anticipates additional cases of monkeypox to be found as surveillance extends in non-endemic countries,” the WHO said, taking note of the issue.
Transmission of Monkeypox and Coronavirus
Monkeypox is caused by the Orthopoxvirus genus, which belongs to the Poxviridae family. It’s a zoonosis caused by a virus (a virus transmitted to humans from animals). This virus can be passed from one person to another and from one animal to another. The infection spreads through broken skin, the respiratory tract, or oral mucosa (even if they are not apparent) (eyes, nose, or mouth).
This happens when you come in contact with droplets in the air from a cough or sneeze. It can also be passed from person to person through close exposure to blood or lesion material. COVID-19 is significantly more transmissible than the monkeypox virus and can spread quickly from one person to another.
According to the World Health Organization, monkeypox cases have been discovered primarily, but not solely, among men who have intercourse with men (MSM) getting treatment in inpatient healthcare and sexual health clinics.
Symptoms of Monkeypox and Coronavirus

A prominent bumpy rash, a temp, chills, painful muscles, malaise, lethargy, and a headache are all signs of monkeypox, which is a disease in the same genus as smallpox. Fever, dry mouth, cough, exhaustion, runny nose, chronic stiffness, headache, difficulty breathing, heart palpitations, loss of taste and smell, and fatigue are all symptoms of the Coronavirus.
Which is a more significant threat: Monkeypox or Coronavirus?
Experts feel that the monkeypox disease is less harmful and deadly than Coronavirus. COVID-19 is more hazardous than the monkeypox virus because it can transmit quickly from one person to the next. Furthermore, whereas COVID-19 includes single threads of genetic code known as RNA, the monkeypox infection has a quintuple genetic code in the form of DNA.
Treatment and Vaccine for Monkeypox and Coronavirus
There are COVID-19 vaccinations on the market. In addition, many patients have received booster doses of the virus. Monkeypox vaccinations, on the other hand, are still unavailable. There is no known therapy for monkeypox, as per the Centers for Disease Control and Prevention (CDC). Still, because monkeypox is connected to smallpox, the smallpox vaccination, antivirals, and vaccinia antibody globulin can protect people against monkeypox.

The World Health Organization (WHO) has noted in reaction to stigmatizing monkeypox material that has been circulating online. Around the outbreak of monkeypox, we’ve seen messages stigmatizing specific categories of people. We want to be sure that this is not acceptable. First and foremost, anyone who comes into direct personal contact with those with monkeypox, independent of who they are, how they do it, who they get to have sex with or any other factor, is in danger.
Second, it is inappropriate to stigmatize somebody because of their condition or disease. Stigma will only exacerbate the situation and prevent us from ending the outbreak as quickly as possible. We must all work together to promote everyone who has been sick or is assisting in caring for sick people. We know how to halt the spread of this sickness and safeguard ourselves and others. Stigmatization is never acceptable, and they certainly aren’t permitted in the context of this outbreak. This is a team effort for all of us.
Edited by Prakriti Arora





