
Just when the world is expecting a third wave of the Coronavirus, China once again decided to scare the world by reporting the first human infection case with Monkey B virus (BV) after a veterinarian based in Beijing was confirmed with Monkey B virus. The news spread worldwide along with panic that this might be next in line to the Corona. According to reports by China CDC, the Beijing based veterinarian was confirmed with the infection a month after he dissected two dead monkeys in March. The veterinarian who died due to the infection, worked for an institution that researched on non-human primates, started experiencing early-onset signs of vomiting and nausea in April.
After the veterinarian’s death in May, China claimed that there were no lethal or even clinically noticeable BV infections in China before. According to China, this case marks the first human infection case with the Monkey B virus. According to records, the virus which was first identified in 1932, has infected only 50 people till 2020 among which only 21 died.
What is the Monkey B virus?
Macacine alphaherpesvirus 1 was initially isolated in 1932 after the death of William Brebner, a young doctor who was bitten by a rhesus monkey. The Monkey B virus or herpes B is found among macaque monkeys, but they are extremely rare and often lethal when spreads to humans. The virus is an alphaherpesvirus enzootic in macaques. Other primates such as chimpanzees and capuchin monkeys, can become infected with it and eventually the infection might cause death. As per the U.S. Centre for Disease Control and Prevention (CDC), there have not been documented cases of such primates spreading the B virus.
Macaques, a genus of Old World monkeys are the natural host. B virus is also commonly known as herpes B, herpes-virus simiae, monkey B virus, and herpes virus B. The Chinese Centre for Disease Control advised that this in monkeys might cause a potential risk to occupational workers.
How is it transmitted?
According to the US CDC, infections in humans due to the B virus is extremely rare and happen only when exposed directly to either the host (macaques) or their body fluids or tissues. The fatality rate of the infection is 70 per cent to 80 per cent. As per CDC, macaque monkeys generally have it and it can be traced in their saliva, urine, faeces, or cerebral or spinal cord fluids or tissue. It can also be found in cells derived from an infected monkey in a laboratory. It is capable of surviving for hours on moist surfaces.
When can a human get infected with a B virus?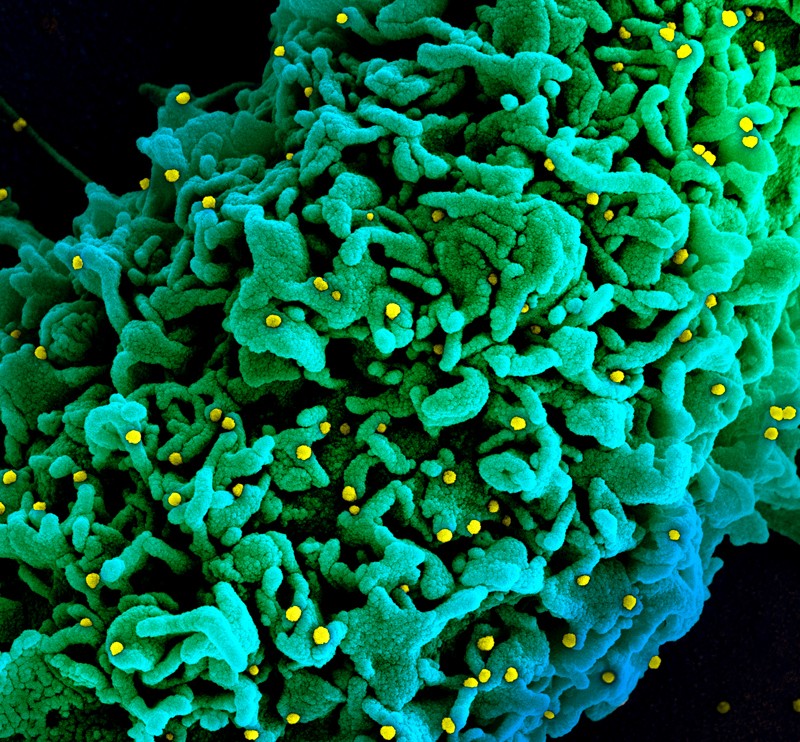
The incubation period of the virus for infection in humans after a positive exposure ranges from 2 days to 5 weeks. According to few well-documented cases, the infection happens within 5 to 21 days. Humans get infected by the virus if they are scratched or bitten by a diseased monkey; if an infected monkey’s fluid or tissue gets inside the human’s body through broken skin, open wound or gets in eyes, nose or mouth; get bruised or cut oneself on an infected monkey’s cage or similar other sharp-edged object or get exposed to the spinal cord, or skull or the brain of an infected monkey.
Symptoms
According to CDC, symptoms are detectable within a month of being exposed it, but can also start within three to seven days. The initial indications of the infection are generally flu-like indications such as fever and shivering, muscle ache, headache and fatigue. After few days of flu-like symptoms, the infected person may develop small blisters near the wound area on the body that came in proximity with the infected monkey. Some other symptoms include nausea, shortness of breath, vomiting, hiccups and abdominal pain.
As the infection progresses, the microbe spreads steadily to the brain and spinal cord, causing inflammation. This is followed by inflammatory and neurologic symptoms like pain, itching near the wound site, numbness; trouble in muscle coordination; respiratory failure; seizures; cranial nerve palsies; ataxia; brain damage and acute damage to the nervous system. In the later stage, the patient generally goes into a coma or dies.
Is there a vaccine?
No. Presently, no vaccines are available that can protect a person against this ifection
Who are at higher risk for getting infected?
Laboratory workers, veterinarians, zookeepers and others who may be exposed to monkeys are at high risk and they have the highest chances of getting infected.
Is human-to-human transmission possible?
To date, only a single case has been recorded of an infected person transmitting it to another person.
Treatment
As there are no vaccines available, the only treatment is fluid therapy and antiviral medicine. For the treatment to be effective, early diagnosis of the infection is crucial.
Kyasanur Forest Disease (KFD)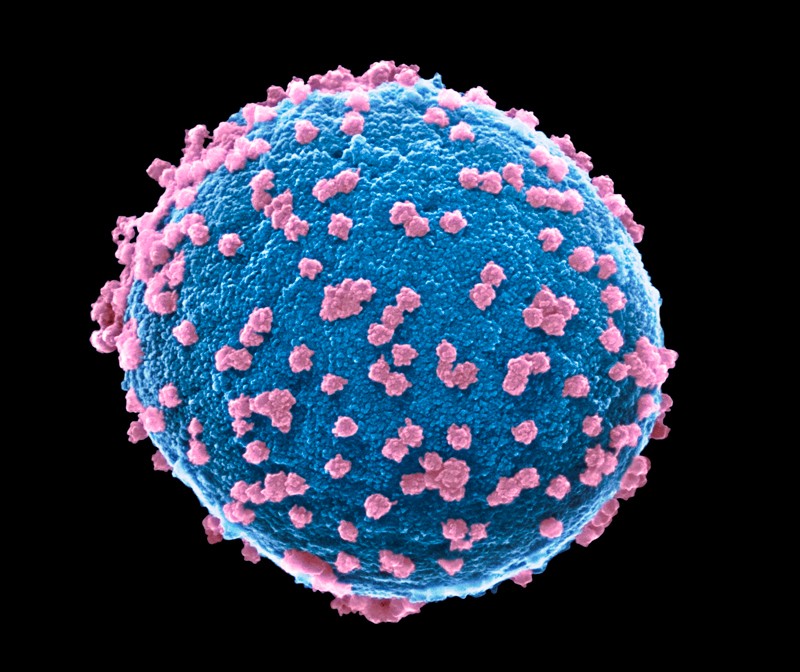
One should not confuse the Monkey B virus with Kyasanur Forest Disease (KFD). KFD is a tick-borne viral disease that is prevalent in the southern state of Karnataka in India. It is also called monkey fever by the locals. The virus responsible for KFD is a member of the genus Flavivirus and the family Flaviviridae. Whereas B virus from family Herpesvirus simiae.
Transmission of the KFD mainly occurs after a tick bite or contact with an infected animal (dead or alive). To date, no person-to-person transmission has been recorded. Animals such as cows, sheep and goats may also become infected with KFD but they play a minimum role in the transmission. These animals serve as the host for ticks that feast on their blood. It is also possible for the diseased animals with viremia to infect other ticks. However, the spreading of KFDV to humans from these animals is highly rare. Also, there is no record of the disease transmission through the unpasteurized milk of any of these animals.




