In 2022, will Omicron end the pandemic?

In 2022, will Omicron end the pandemic?
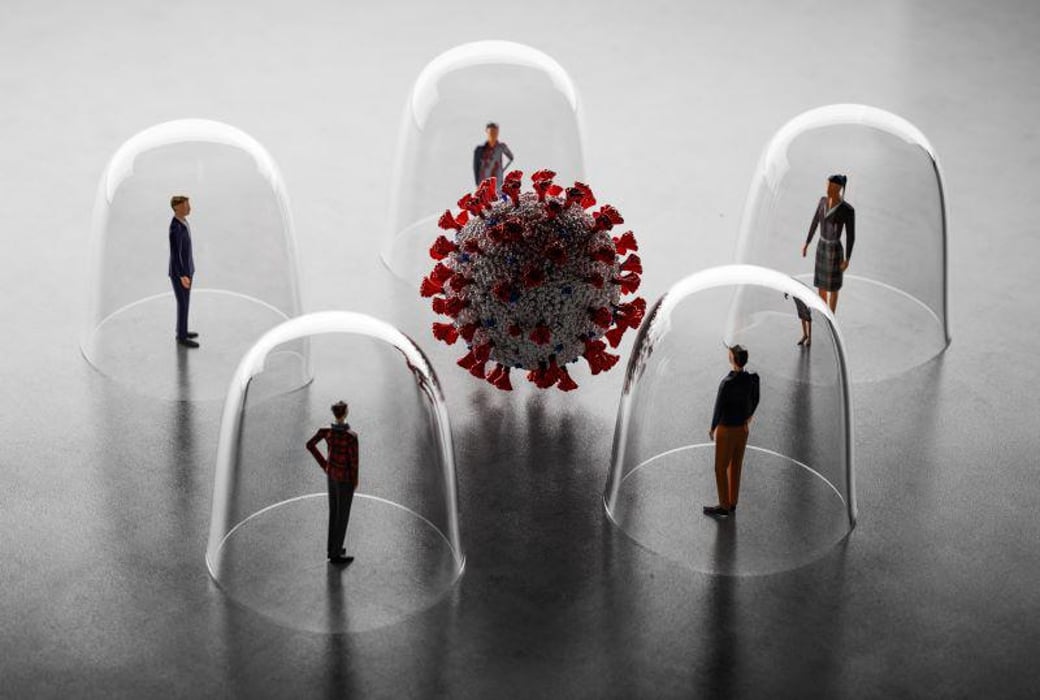
Various vaccine strategies, the rapid spread of the variant, and varying immunity levels make modelling the pandemic’s future challenging. Health officials from the World Health Organization (WHO) warned of a disease tidal wave from west to east on 11 January, seven weeks after the Omicron variant was first reported. The WHO’s regional director for Europe, Hans Henri Kluge, said 50 out of 53 countries in Europe and Central Asia had reported cases of Omicron.
Various factors will affect how countries cope with pandemics, including their epidemiological circumstances, the availability of resources, vaccination uptake rates and socioeconomic conditions. As of earlier this month, more than 160,000 COVID-19 cases per day have been reported in the United Kingdom, the country that has reported most Omicron infections. The problem all nations face is spreading the variants at a fast rate.
The COVID-19 and Omicron virus is not harmless even though it is endemic
Though the WHO argues that a surge in Omicron infections could signal the end of the pandemic, researchers warn that things remain erratic and hard to predict because of the short-term immunity boost that will follow.
“It rushes that it presents a short window of opportunity to respond. The government must make decisions under huge uncertainty,” says Graham Medley, an infectious-disease modeller at the London School of Hygiene & Tropical Medicine.
- Modelling is difficult
In the beginning, UK modellers were unsure whether they should use South African information. A computer model can easily be updated to account for changes in a new variant’s biological properties.
As the pandemic has progressed, it has become increasingly difficult to predict how a country’s immune response will affect spreading.
Since COVID-19 was a newly diagnosed disease and no vaccine was available at the time, researchers expected most people worldwide to be equally susceptible. After 12 months of distinct vaccine strategies, types, and take-up rates from country to country, and fluctuating rates of infection and recovery, the immunological landscape is becoming increasingly diverse.
It is crucial to consider the probability of infection leading someone to the hospital. The University of Edinburgh’s infectious-disease epidemiologist Mark Woolhouse, who advises the UK government, says that number is now being estimated in a population that isn’t naive. It’s best to remake those sorts of estimates for every population that you’re interested in when you make those estimations, and that goes for everywhere.
- Vaccination differences
There isn’t much specific information about reduced severity in the South African data, which confused modellers. Woolhouse says no quantitative analysis was done. So, what numbers should I input? Which is less pathogenic, 10% less, 50% less, or 90% less?”
In any case, Woolhouse, speaking for himself, argues that some influential modellers in the United Kingdom were wrong not to allow for a reduction in severity, instead of carrying out simulations assuming Omicron hospitalization rates identical to those of comparable variants. He believes that in a pessimistic way.
Having made a clear statement in the beginning that there was an option for less pathogenicity and being crystal clear about what the implications of those differences might would have been helpful.”
Omicron is difficult to predict with any degree of precision because of the heterogeneity in immunological baselines among countries and the differences in population dynamics within individual countries. Moreover, it is difficult to predict how the variant might spread in countries with lower vaccination rates. Virologist Julian Tang, who works at the Leicester Royal Infirmary in the UK, says he cannot answer that question.
It is spreading in pattern XYZ across western Europe, ABC across North America, and MNO in Africa does not help anyone in the long run.
- Spreading rapidly
Public health officials would expect Omicron infections to double in less than two days since it is significantly faster than prior SARS-CoV-2 variants. A scientist compared Omicron to the flu on acid.
Christina Pagel, a healthcare data analyst at University College London, says her team has never seen such a speed before, and she tells us you can’t vaccinate your way out of it. Even if everyone were vaccinated, the vaccine would take two weeks to take effect, and by then, you would already be affected by the disease.”
Researchers and policymakers are therefore placed in a difficult position. In Pagel’s opinion, you had two choices: Either put in the restrictions very early or don’t. But if you wait, the damage will be done already.
In December, Britain tightened regulations along with other countries. Nevertheless, the move was controversial, especially considering reports from South Africa, which had been sickened by Omicron the month before, that the variant had been causing less severe illness and hospitalization than the original strain – a conclusion now backed up by Britain’s experience.
- Waning protection
In addition, vaccines against Omicron offer a diminishing degree of protection against infection. There are few antibodies to the variant elicited by inactivated-virus vaccines, which comprise almost half of the ten billion doses distributed worldwide. Omicron will be able to rip through places that rely on these shots even more quickly, then? The answer is no, says Woolhouse.
Because of the limited amount of real-world data, this is the case. Pagel explains that they are only hitting countries that have used them.
Omicron has made the most progress in the Philippines, where COVID-19 cases have risen exponentially this month, particularly in Manila, among countries that rely on these vaccines. It appears that the number of new infections is declining in the capital, but the virus has spread nationwide. According to Maria Rosario Vergeire, health spokesperson for the Philippine government, “Cases have definitely slowed down in the [National Capital Region], but in other regions, they are now increasing.”
Only 53% of the Philippines’ population is fully vaccinated, which is relatively low. According to officials, vaccines are to be given to all 77 million adults by the end of May.
It’s unlikely that vaccines will continue to prevent severe symptoms, but the spread of infection will persist. It assumes that none of the vaccines will prevent infection for a long time.
“Vaccines are not going to be the solution to this pandemic,” says Tang.
When will it end?

What will be the outcome? Researchers predict it won’t be Omicron. Medley says next year’s variant will have its characteristics since it won’t last.
According to scientists, COVID-19 will become an endemic disease if not completely disappear. There are many different interpretations of that concept, and its significance can vary from person to person. A London School of Hygiene & Tropical Medicine epidemiologist, Sebastian Funk, believes that the general expectation is that we would no longer see deadly epidemics if populations had so much immunity.
As he adds, it is difficult to model with any precision the process of becoming an endemic or living with the virus without restrictions and safeguards. The reasons are partly because even the best disease models do not make accurate forecasts beyond a few weeks. Moreover, endemicity reflects the number of deaths societies are willing to tolerate while immunity is steadily building up in the global population.
Woolhouse believes that COVID-19 can only become endemic once most adults are protected from serious infection due to their exposure to the virus as children. Therefore they have a natural immunity to it. It will take decades, and many older people today won’t benefit from vaccinations since they haven’t been exposed to the virus as children.
There are flaws in that strategy. Exposure to COVID as a child can result in long-term health effects. As variants evolve, the rates of severe illness must continue to fall among children.
Tang says there is no guarantee that the next variant will be milder, but it seems to have been that way so far. Upon repeated exposure, the virus becomes milder.
The COVID-19 virus is not harmless even though it is endemic
One of the most misunderstood terms in the pandemic has become endemic. Erroneous assumptions have contributed to a complacent attitude. COVID-19 will not end naturally as a result of this decision.
Epidemiologists define an endemic infection in which overall rates are static – not increasing nor decreasing. More precisely, it implies that as long as everyone gets sick, the proportion of infected people balances out the ‘basic reproduction number’ of the virus, or how many people an infected individual would infect.
The common cold is an endemic disease, and malaria, Lassa fever, and polio are also endemic diseases. Smallpox, until it was eradicated, is also endemic.
An endemic disease can be widespread and deadly at the same time. More than 600,000 people died of malaria in 2020, and one and a half million people died from tuberculosis that year. The word epidemic does not mean evolution has somehow tamed a pathogen to the point where life can return to a more ‘normal’ state.
The word endemic is invoked as an excuse by policymakers to do nothing or little when I am an evolutionary virologist—learning to live with endemic diseases such as measles, rotavirus, or hepatitis C aren’t the only aspects of global health policy.
It is impossible to judge how long it will take infection to become endemic, the case rates, mortality rates or morbidity rates, or what proportion of a population will be affected. As the US measles outbreak in 2019 demonstrated, there can still be waves of disruption from endemic infections. Out of many possible forms, endemic COVID-19 will take on the form determined by health policies and individual behaviour.
Alpha’s emergence and spread in late 2020 prompted my analysis of how, unless infections are suppressed, viral evolution would be fast and unpredictable, resulting in more variants with different and potentially more-damaging biological characteristics.
After that, public-health systems struggled with the highly transmissible and virulent Delta strain, and now Omicron has emerged, with its substantial ability to evade an immune system, causing reinfection and outbreaks. In addition to Beta and Gamma, both were highly dangerous, but they were not as widespread.
The interplay between a population’s behaviour, demographic structure, susceptibility and immunity, and the emergence of virus variants determines whether a virus causes endemic, epidemic or pandemic infection. Varieties can evolve under different conditions around the world, and each can generate a new outbreak. Regions’ ability to respond to infections is tied to their policy decisions.
A region might reach an equilibrium – whether it is of low disease and death or one of high disease and death – but that equilibrium may be disturbed when a new variant appears.
The COVID-19 pandemic, although severe, is not the first in history. Evolutionary battles with infection have led our immune systems to evolve to cope with constant infections, and the genetic material from ancient viral infections is embedded in our genomes as a remnant of such evolutionary struggles. Some viruses may have died out on their own and still caused high mortality rates before going extinct.
The belief that viruses will become benign with time is widespread and rosy. Viruses such as SARS-CoV-2, which is transmitted before it causes major illness, cannot automatically become more benign. Unlike the first discovered strain in Wuhan, China, Alpha and Delta are more virulent strains. During the 1918 influenza pandemic, the second wave was far more deadly than the first.

Evolutionary arms races can be changed in humanity’s favour much more easily than most people think. The first step is to stop being so optimistic. Third, we must be realistic about the level of death, disability, and illness that we can expect. Reduction targets should consider the risk of new virus variants arising from circulating viruses.
Fourth, we must use all available weapons against airborne diseases: vaccines, antiviral medications, diagnostic tests, and solutions like masks, distance, air filtration, and ventilation. The fourth thing we must do is invest in vaccines that protect against a wider range of variations.
It requires a variety of integrated public health interventions to prevent the spread of new, more-damaging and more-transmissible variants, including, crucially, vaccine equity, to stop the unconstrained spread. Viruses that reproduce more frequently are more likely to generate problematic variants, most likely where the spread is greatest. Omicron and Delta were identified first in southern Africa after Alpha was found in the United Kingdom.
As well as being wrong, thinking that endemicity is quite dangerous, as it sets humanity up for many more years of disease, including unpredictable outbreaks. We would be better off considering the consequences of keeping giving the virus changes to outwit us if we keep giving it chances. That way, we might be able to prevent this from happening.
Edited and published by Ashlyn Joy




